Michael Eisenstein in Nature:
 The treatment was never going to work. Ryan Corcoran, an oncologist at Massachusetts General Hospital, Boston, didn’t realize this when he began treating his patient’s colorectal cancer in 2014. His team picked a therapy on the basis of genetic testing of a portion of the person’s cancer, and initially the treatment performed well. But before long, it faltered amid overwhelming tumour resistance. It was only when the person had a liquid biopsy, a test based on analysis of stray tumour DNA in the blood, that Corcoran learnt why the treatment the team had selected was doomed to failure. “There was a mutation known to cause resistance to that drug, which wasn’t present in the tissue biopsy but was fairly abundant in the blood sample,” he says. “If we had just biopsied a different lesion, we might’ve picked an entirely different therapy.” The experience demonstrated the benefits of searching the blood for answers. Now, blood-based biopsies are commonplace at his hospital, and are increasingly used in cancer centres around the world.
The treatment was never going to work. Ryan Corcoran, an oncologist at Massachusetts General Hospital, Boston, didn’t realize this when he began treating his patient’s colorectal cancer in 2014. His team picked a therapy on the basis of genetic testing of a portion of the person’s cancer, and initially the treatment performed well. But before long, it faltered amid overwhelming tumour resistance. It was only when the person had a liquid biopsy, a test based on analysis of stray tumour DNA in the blood, that Corcoran learnt why the treatment the team had selected was doomed to failure. “There was a mutation known to cause resistance to that drug, which wasn’t present in the tissue biopsy but was fairly abundant in the blood sample,” he says. “If we had just biopsied a different lesion, we might’ve picked an entirely different therapy.” The experience demonstrated the benefits of searching the blood for answers. Now, blood-based biopsies are commonplace at his hospital, and are increasingly used in cancer centres around the world.
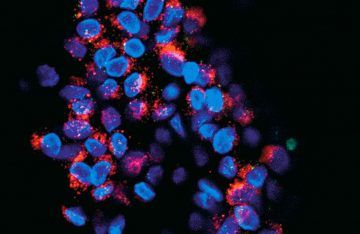
For some cancers, such as advanced non-small-cell lung carcinoma, physicians in Europe and the United States already rely on liquid biopsies to spot the genetic markers that can forecast response or resistance to certain drugs. But oncologists still think there is vast untapped potential in the tests. Catherine Alix-Panabières, a cancer biologist at the University Medical Centre of Montpellier in France, says that liquid biopsies can give a more comprehensive profile of both primary tumours and metastases than can samples harvested directly from the cancer. This is particularly true in tricky tissues such as the brain, where taking a biopsy is extremely difficult, but also for more commonplace tumours of the prostate or breast. “If you don’t put the needle in just the right place, you may miss some important tumour cells,” Alix-Panabières says. Blood sampling could also help clinicians to monitor tumours over the course of treatment, to get advance warning of recurrence or even to predict cancer in seemingly healthy people, well before the onset of symptoms.
“We are just scratching the surface of what we will ultimately be able to do,” says Maximilian Diehn, a radiation oncologist at Stanford University in California. But to get there, researchers still need to show that promising proof-of-concept results can be translated into interventions that provide better clinical outcomes.
More here.
