Kai Kupferschmidt and Jon Cohen in Science:
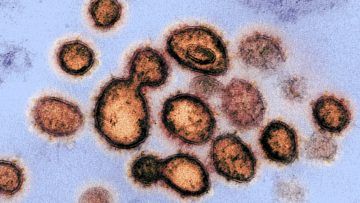 Drugs that slow or kill the novel coronavirus, called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), could save the lives of severely ill patients, but might also be given prophylactically to protect health care workers and others at high risk of infection. Treatments may also reduce the time patients spend in intensive care units, freeing critical hospital beds. Scientists have suggested dozens of existing compounds for testing, but WHO is focusing on what it says are the four most promising therapies: an experimental antiviral compound called remdesivir; the malaria medications chloroquine and hydroxychloroquine; a combination of two HIV drugs, lopinavir and ritonavir; and that same combination plus interferon-beta, an immune system messenger that can help cripple viruses. Some data on their use in COVID-19 patients have already emerged—the HIV combo failed in a small study in China—but WHO believes a large trial with a greater variety of patients is warranted.
Drugs that slow or kill the novel coronavirus, called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), could save the lives of severely ill patients, but might also be given prophylactically to protect health care workers and others at high risk of infection. Treatments may also reduce the time patients spend in intensive care units, freeing critical hospital beds. Scientists have suggested dozens of existing compounds for testing, but WHO is focusing on what it says are the four most promising therapies: an experimental antiviral compound called remdesivir; the malaria medications chloroquine and hydroxychloroquine; a combination of two HIV drugs, lopinavir and ritonavir; and that same combination plus interferon-beta, an immune system messenger that can help cripple viruses. Some data on their use in COVID-19 patients have already emerged—the HIV combo failed in a small study in China—but WHO believes a large trial with a greater variety of patients is warranted.
Enrolling subjects in SOLIDARITY will be easy. When a person with a confirmed case of COVID-19 is deemed eligible, the physician can enter the patient’s data into a WHO website, including any underlying condition that could change the course of the disease, such as diabetes or HIV infection. The participant has to sign an informed consent form that is scanned and sent to WHO electronically. After the physician states which drugs are available at his or her hospital, the website will randomize the patient to one of the drugs available or to the local standard care for COVID-19. “After that, no more measurements or documentation are required,” says Ana Maria Henao Restrepo, a medical officer at WHO’s Department of Immunization Vaccines and Biologicals. Physicians will record the day the patient left the hospital or died, the duration of the hospital stay, and whether the patient required oxygen or ventilation, she says. “That’s all.”
More here.
