Siddhartha Mukherjee in The New York Times:
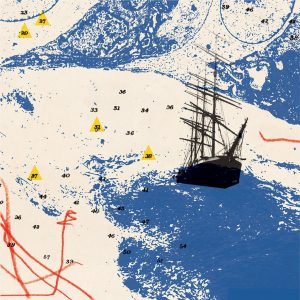 On my way to a meeting on cancer and personalized medicine a few weeks ago, I found myself thinking, improbably, of the Saul Steinberg New Yorker cover illustration “View From Ninth Avenue.” Steinberg’s drawing (yes, you’ve seen it — in undergraduate dorm rooms, in subway ads) depicts a mental map of the world viewed through the eyes of a typical New Yorker. We’re somewhere on Ninth Avenue, looking out toward the water. Tenth Avenue looms large, thrumming with pedestrians and traffic. The Hudson is a band of gray-blue. But the rest of the world is gone — irrelevant, inconsequential, specks of sesame falling off a bagel. Kansas City, Chicago, Las Vegas and Los Angeles are blips on the horizon. There’s a strip of water denoting the Pacific Ocean, and faraway blobs of rising land: Japan, China, Russia. The whole thing is a wry joke on self-obsession and navel gazing: A New Yorker’s world begins and ends in New York.
On my way to a meeting on cancer and personalized medicine a few weeks ago, I found myself thinking, improbably, of the Saul Steinberg New Yorker cover illustration “View From Ninth Avenue.” Steinberg’s drawing (yes, you’ve seen it — in undergraduate dorm rooms, in subway ads) depicts a mental map of the world viewed through the eyes of a typical New Yorker. We’re somewhere on Ninth Avenue, looking out toward the water. Tenth Avenue looms large, thrumming with pedestrians and traffic. The Hudson is a band of gray-blue. But the rest of the world is gone — irrelevant, inconsequential, specks of sesame falling off a bagel. Kansas City, Chicago, Las Vegas and Los Angeles are blips on the horizon. There’s a strip of water denoting the Pacific Ocean, and faraway blobs of rising land: Japan, China, Russia. The whole thing is a wry joke on self-obsession and navel gazing: A New Yorker’s world begins and ends in New York.
In the mid-2000s, it felt to me, at times, as if cancer medicine were viewing the world from its own Ninth Avenue. Our collective vision was dominated by genomics — by the newfound capacity to sequence the genomes of cells (a “genome” refers to the complete set of genetic material present in an organism or a cell). Cancer, of course, is typically a disease caused by mutant genes that drive abnormal cellular growth (other features of cellular physiology, like the cell’s metabolism and survival, are also affected). By identifying the mutant genes in cancer cells, the logic ran, we would devise new ways of killing the cells. And because the exact set of mutations was unique to an individual patient — one woman’s breast cancer might have mutations in 12 genes, while another breast cancer might have mutations in a different set of 16 — we would “personalize” cancer medicine to that patient, thereby vastly increasing the effectiveness of therapy.
This kind of thinking had an exhilarating track record. In the 2000s, a medicine called Herceptin was shown to be effective for women with breast cancer, but only if the cancer cells carried a genetic aberration in a gene called HER-2. Another drug, Gleevec, worked only if the tumor cells had a mutant gene called BCR-ABL, or a mutation in a gene called c-kit. In many of our genome-obsessed minds, the problem of cancer had become reduced to a rather simple, scalable algorithm: find the mutations in a patient, and match those mutations with a medicine. All the other variables — the cellular environment within which the cancer cell was inescapably lodged, the metabolic and hormonal milieu that surrounded the cancer or, for that matter, the human body that was wrapped around it — might as well have been irrelevant blobs receding in the distance: Japan, China, Russia.
