From Nature:
 It seemed like a very promising cancer immunotherapy lead. CHO Pharma, in Taiwan, had discovered that it was possible to target solid tumours with an antibody against a cell-surface glycolipid called SSEA-4.1 This antigen is present during embryonic development, but not seen on human cells again — until they turn into cancer cells.2 The company turned to Lan Bo Chen, a recently retired Harvard pathologist, to help develop this work into an anti-cancer therapy for solid tumours. “It is highly reasonable to imagine that we can use SSEA-4, overexpressed on cancer cells, as a target for CAR-T,” says Chen, now in his role as senior technology advisor for CHO Pharma.
It seemed like a very promising cancer immunotherapy lead. CHO Pharma, in Taiwan, had discovered that it was possible to target solid tumours with an antibody against a cell-surface glycolipid called SSEA-4.1 This antigen is present during embryonic development, but not seen on human cells again — until they turn into cancer cells.2 The company turned to Lan Bo Chen, a recently retired Harvard pathologist, to help develop this work into an anti-cancer therapy for solid tumours. “It is highly reasonable to imagine that we can use SSEA-4, overexpressed on cancer cells, as a target for CAR-T,” says Chen, now in his role as senior technology advisor for CHO Pharma.
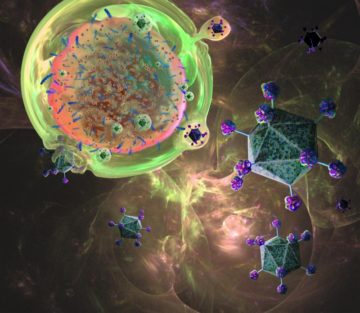
CAR-T therapy works by genetically engineering a person’s own T cells in such a way that they recognize and attack cancer cells. This involves creating a chimeric antigen receptor (CAR) from an antibody against a target on the cell. But CAR-T therapy was designed for blood cancers so it needs several adaptations to make it suitable for the treatment of solid tumours.3 The cells need to be directed to the site of the tumour, survive in the tumour’s local microenvironment, and act only on tumour cells, not on healthy cells nearby.
But, when Chen tried to create CAR-T cells against SSEA-4, he hit a few obstacles. First it took him a long time to get his hands on a humanized SSEA-4 antibody suitable for adaptation. When he finally had one, he still had to find a way to turn that antibody into a CAR. And then to insert the CAR into a human T cell using lentiviral transduction.
More here.
