Sarah DeWeerdt in Nature:
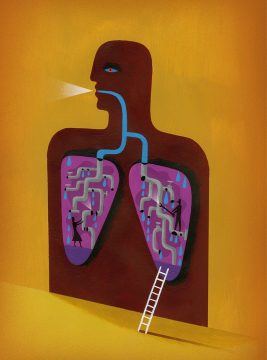 Over the course of two decades spent developing treatments for the genetic lung disease cystic fibrosis, biologist Fredrick Van Goor has had hundreds of conversations with patients. But he remembers one in particular. The discussion was about the genetics of cystic fibrosis, a disease that develops when a person inherits two faulty copies of the cystic fibrosis transmembrane conductance regulator (CFTR) gene. This gene encodes the CFTR protein, which resides in the cell membrane and transports chloride and bicarbonate ions out of the cell. More than 2,000 variants of CFTR have been identified, and more than 350 of them are known to produce enough disruption in the protein’s function to trigger the debilitating and life-shortening condition. The focus of the conversation was the inevitable inequities of personalized medicine, which can be highly effective for people who meet certain criteria, but will leave others behind — as was the case for this patient. “He described it as being on a sinking ship, when all of the other lifeboats have left,” Van Goor recalls. “That image has stuck with me.”
Over the course of two decades spent developing treatments for the genetic lung disease cystic fibrosis, biologist Fredrick Van Goor has had hundreds of conversations with patients. But he remembers one in particular. The discussion was about the genetics of cystic fibrosis, a disease that develops when a person inherits two faulty copies of the cystic fibrosis transmembrane conductance regulator (CFTR) gene. This gene encodes the CFTR protein, which resides in the cell membrane and transports chloride and bicarbonate ions out of the cell. More than 2,000 variants of CFTR have been identified, and more than 350 of them are known to produce enough disruption in the protein’s function to trigger the debilitating and life-shortening condition. The focus of the conversation was the inevitable inequities of personalized medicine, which can be highly effective for people who meet certain criteria, but will leave others behind — as was the case for this patient. “He described it as being on a sinking ship, when all of the other lifeboats have left,” Van Goor recalls. “That image has stuck with me.”
Van Goor, the head of cystic fibrosis research at Vertex Pharmaceuticals in San Diego, California, had a major role in building the biggest lifeboat for cystic fibrosis yet: the blockbuster combination drug Trikafta. The drug achieved sales of US$420 million in the first 10 weeks after its launch in late 2019, far exceeding expectations. “I think it has made a big difference,” says Martina Gentzsch, a molecular biologist studying CFTR at the University of North Carolina at Chapel Hill. “The success in the clinic really justifies that this is an absolutely outstanding treatment.” Trikafta is indicated for people with cystic fibrosis who carry at least one copy of a mutation known as F508del. This is the most common cystic fibrosis mutation, present in more than 80% of the over 90,000 people with cystic fibrosis worldwide.
More here.
