 Jonathan Fuller in Boston Review:
Jonathan Fuller in Boston Review:
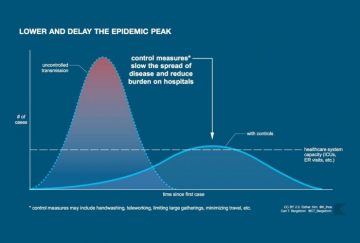
The lasting icon of the COVID-19 pandemic will likely be the graphic associated with “flattening the curve.” The image is now familiar: a skewed bell curve measuring coronavirus cases that towers above a horizontal line—the health system’s capacity—only to be flattened by an invisible force representing “non-pharmaceutical interventions” such as school closures, social distancing, and full-on lockdowns.
How do the coronavirus models generating these hypothetical curves square with the evidence? What roles do models and evidence play in a pandemic? Answering these questions requires reconciling two competing philosophies in the science of COVID-19.
In one camp are infectious disease epidemiologists, who work very closely with institutions of public health. They have used a multitude of models to create virtual worlds in which sim viruses wash over sim populations—sometimes unabated, sometimes held back by a virtual dam of social interventions. This deluge of simulated outcomes played a significant role in leading government actors to shut borders as well as doors to schools and businesses. But the hypothetical curves are smooth, while real-world data are rough. Some detractors have questioned whether we have good evidence for the assumptions the models rely on, and even the necessity of the dramatic steps taken to curb the pandemic. Among this camp are several clinical epidemiologists, who typically provide guidance for clinical practice—regarding, for example, the effectiveness of medical interventions—rather than public health.
More here.
